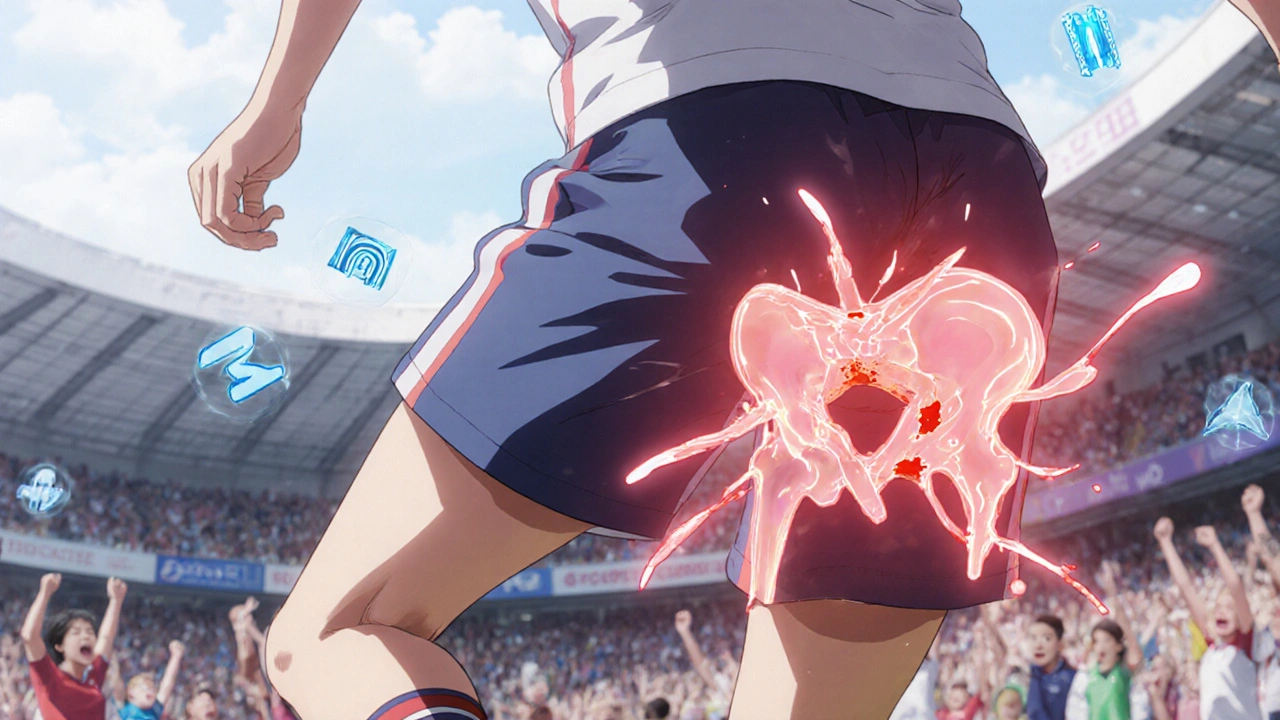
What Exactly Is a Hip Labral Tear?
A hip labral tear happens when the ring of cartilage (the labrum) that surrounds the hip socket gets damaged. This cartilage acts like a seal, keeping the ball of the femur snug in the socket. When it tears, you don’t just get pain-you get instability, clicking, locking, and a deep ache in the groin or buttock that gets worse with movement. It’s not a simple strain. This is structural damage, and for athletes, it can end seasons-or careers-if not handled right.
It’s not rare. About 1 in 4 athletes with persistent hip pain have a labral tear. Basketball players, soccer midfielders, hockey forwards, and distance runners are most at risk. Why? Because their hips are constantly twisting, flexing, and rotating under load. Over time, this wears down the labrum. But the real culprit behind most of these tears isn’t just overuse-it’s femoroacetabular impingement (FAI). That’s when the bones of the hip are shaped abnormally, causing them to rub against each other like sandpaper. FAI is the root cause in up to 80% of cases in young athletes.
How Do You Know It’s a Labral Tear and Not Just a Pull?
Most athletes write off hip pain as a muscle strain. But a labral tear doesn’t heal with rest and ice alone. You’ll notice specific signs: pain when you squat, sit for long periods, or twist your hip. The classic test? The FADIR maneuver-flex your hip to 90 degrees, pull your knee toward your chest, then rotate it inward. If that triggers sharp pain in the groin, it’s a red flag. The FABER test (flex, bend, rotate outward) can also reproduce symptoms. These tests aren’t perfect, but they’re accurate in nearly 80% of confirmed cases.
What makes it tricky is that other conditions mimic it. Athletic pubalgia, hip bursitis, even sciatica can feel the same. That’s why jumping straight to an MRI isn’t enough. The first step is always X-rays. They check for bone deformities like FAI, hip dysplasia (a shallow socket), or early arthritis. If those look normal but symptoms persist, you move to imaging that actually sees soft tissue.
Why MRA Is the Gold Standard for Diagnosis
Standard MRI misses up to 30% of labral tears. Why? Because the labrum is small, dense cartilage, and without contrast, tears blend into surrounding tissue. That’s where magnetic resonance arthrography (MRA) comes in. This isn’t just an MRI with dye-it’s an MRI after injecting contrast directly into the hip joint. The fluid expands the joint space, making even tiny frays and partial tears stand out like cracks in glass.
MRA isn’t perfect, but it’s the best non-surgical tool we have. It catches 90-95% of labral tears and correctly rules them out 85-92% of the time. That’s why top sports medicine centers require it before considering surgery. A 2023 multicenter study showed that 3D MRA sequencing improved accuracy to 97% in complex cases. Without it, you risk misdiagnosing a tear as simple inflammation-or worse, missing a tear entirely and letting it worsen.
Cost is a barrier. A standard MRI runs $500-$800. MRA? $1,200-$1,800. Many athletes pay out of pocket because insurance won’t cover it unless conservative treatment fails first. But skipping MRA is like trying to fix a car engine without opening the hood.
When Arthroscopy Isn’t Just a Treatment-It’s a Diagnosis
Even MRA can’t show everything. That’s why hip arthroscopy remains the gold standard. It’s not just a surgical fix-it’s the only way to see the labrum with your own eyes. During the procedure, a tiny camera is inserted through a small incision. Surgeons can see exactly where the tear is, how big it is, and whether there are loose fragments or cartilage damage nearby. Accuracy? Nearly 98%.
But here’s the catch: arthroscopy isn’t always about fixing the tear. Sometimes, it’s about finding out what’s really wrong. In 40% of cases, surgeons find additional problems-synovitis, loose bodies, or cartilage wear-that imaging missed. That’s why some athletes get diagnosed with a labral tear, have surgery, and still hurt afterward. The root issue wasn’t the labrum-it was something else.

Conservative Treatment: Does It Work?
Not every labral tear needs surgery. For mild cases, especially in older athletes or those with low-impact lifestyles, conservative care can help. The standard protocol: 4-6 weeks of rest, avoiding deep squats and twisting motions, plus NSAIDs like ibuprofen or naproxen to reduce swelling. Physical therapy is often added, but results are mixed.
Studies show only 30-40% of athletes fully recover with conservative treatment alone. But newer data from True Sports Physical Therapy suggests 65% can manage symptoms without surgery-especially if therapy targets core stability, hip mobility, and neuromuscular control. The key isn’t just strengthening the hip-it’s retraining how the whole body moves. If your glutes are weak, your hip takes the strain. If your pelvis tilts forward, your labrum gets pinched.
Corticosteroid injections can buy time. They reduce inflammation and give 70-80% of patients relief for 3-6 months. But they don’t heal the tear. They just quiet the noise. Use them as a diagnostic tool: if the injection helps, the pain is coming from the joint. If it doesn’t, look elsewhere.
When Surgery Becomes Necessary
If pain lasts more than 3-6 months despite conservative care, surgery is the next step. The two main options: debridement (trimming the torn part) or repair (reattaching the labrum with sutures). Which one you get depends on the tear’s location, size, and quality of the tissue.
Debridement is quicker. Recovery is 3-4 months. But it’s not a long-term fix if the underlying cause-like FAI or dysplasia-isn’t addressed. The American Academy of Orthopaedic Surgeons warns that isolated debridement leads to 40% higher revision rates. Repair is more involved. It takes 5-6 months to recover. But if the labrum is healthy enough to stitch back, it’s the better option. It preserves the joint’s seal, which reduces long-term arthritis risk.
And if you have hip dysplasia? Then repair alone isn’t enough. You need a procedure to deepen the socket-like a periacetabular osteotomy. Without fixing the bone structure, the labrum will tear again. Studies show 60-70% re-tear rates in dysplastic hips if the bone isn’t corrected.
Recovery and Return to Sport: What to Expect
Recovery isn’t just about waiting for pain to go away. It’s about rebuilding strength, control, and movement patterns. A typical rehab plan has four phases:
- Protection (Weeks 1-6): No weight-bearing twists. Use crutches if needed. Gentle range-of-motion exercises.
- Strengthening (Weeks 7-12): Focus on glutes, hamstrings, core. Avoid deep hip flexion.
- Sport-Specific Training (Weeks 13-20): Agility drills, controlled cutting, jumping. Progress slowly.
- Return to Sport (Weeks 21-26): Only when you hit 90% quadriceps strength symmetry and can rotate your hip inward to 30 degrees without pain.
Professional athletes like NHL player Ryan Nugent-Hopkins took 5.5 months to return. Amateur runners reported full recovery at 4.5 months with strict rehab. But those who rushed back-often because of insurance pressure or team demands-had higher re-injury rates.

What Can Go Wrong?
Complications are rare but real. About 15-20% of patients still have pain after surgery. Heterotopic ossification-bone growing where it shouldn’t-happens in 5-10%. Nerve injury, though uncommon (1-2%), can cause numbness or tingling down the leg. Revision surgery is needed in 8-12% of cases within five years.
The biggest risk? Not addressing the root cause. If you fix the labrum but leave FAI or dysplasia untouched, you’re just delaying the next tear. That’s why top surgeons don’t just repair-they correct. And they use the latest tools: FDA-approved bioabsorbable anchors (like Smith & Nephew’s BioX) that dissolve over time, reducing long-term irritation.
The Bigger Picture: Preventing Osteoarthritis
A labral tear isn’t just a sports injury. It’s a warning sign. A 15-year study found untreated labral tears increase the risk of hip osteoarthritis by 4.5 times within a decade. That’s why early, accurate diagnosis and proper treatment aren’t just about getting back on the field-they’re about keeping your hip functional for life.
Regenerative medicine is starting to play a role. PRP injections showed promise in a 2022 trial, helping 55% of patients avoid surgery. But it’s not magic. It works best as a bridge-giving the body time to heal while you fix movement flaws.
Final Takeaway: Don’t Guess. Get the Right Scan.
If you’re an athlete with persistent hip pain, don’t assume it’s a strain. Don’t settle for a standard MRI if your symptoms don’t improve. Demand MRA. Ask about FAI and dysplasia. Push for a surgeon who specializes in hip arthroscopy-not just any orthopedist. The difference between a good outcome and a failed one often comes down to one thing: precision. And precision starts with the right diagnosis.

Comments
I've had two labral tears and honestly the MRA was the only thing that showed the full extent. Standard MRI said 'mild degeneration' - turned out it was a full-thickness tear with a loose body. Don't skip the contrast. Took me 6 months to get back to running but worth it.
biggest thing no one talks about is how weak your glutes have to be for this to happen. i did 3 months of physio focusing only on clamshells and hip thrusts and the pain just vanished. no surgery needed.
Typical American overmedicalization. Just stop playing sports if your hip hurts. No one in my village in Nigeria ever heard of a labral tear until they got a visa to the US.
The assertion that MRA is the gold standard for diagnosis is not universally supported in the literature. A 2021 meta-analysis in the Journal of Orthopaedic Research suggests that high-resolution ultrasound, when performed by a skilled operator, demonstrates comparable sensitivity.
Just had my second hip scope last month. Dude the recovery is brutal but 100% worth it. I’m back on the court and my quad strength is actually better than before 😎
As someone from India who trained in athletics for 12 years, I can say this: we never had access to MRA or arthroscopy. We just rested, did yoga, and avoided deep squats. Many of us played through pain and lived fine. Modern medicine is great but sometimes simpler is better.
I was told I needed surgery after my first MRI. Got a second opinion, did 8 weeks of PT, and now I run 5Ks without pain. Sometimes the system pushes surgery because it’s profitable, not because it’s necessary.
If you're reading this and you're an athlete with hip pain, please don't ignore it. I waited 11 months thinking it was a strain. By the time I got the MRA, the tear was massive. You owe it to your future self to get it checked properly.
This whole article is just corporate orthopedics propaganda. Why not just tell people to stop overtraining? Why push expensive scans and surgery? In my country we use turmeric paste and rest. No one needs a $1800 scan to know when to stop pushing.
The author exhibits a distressing tendency toward technocratic reductionism, wherein the complex biomechanical phenomenology of human movement is reduced to a series of diagnostic algorithms and procedural interventions. One cannot help but lament the erosion of holistic medical philosophy in favor of commodified orthopedic spectacle.
This is why America is weak. We turn every little ache into a crisis. In my dad’s time, you played through pain. Now kids get MRIs for a twinge. We need to stop coddling athletes and make them tough again.
I'm not a doctor, but I've read a lot. And I think the most important thing here is that FAI is the root cause in 80% of cases - so if you're getting labral tears, you need to be evaluated for FAI, not just the tear. That's the real key.
Just got my MRA results back - full-thickness tear + FAI. Surgery scheduled in 3 weeks. If anyone’s going through this, DM me. I’ll send you my rehab plan. You got this 💪
Wait so if you have FAI and you don't get surgery, does that mean you're just gonna be in pain forever? I'm 28 and I play soccer on weekends. I don't want to quit but I don't want to be old and broken either.